Between the 4th and the 14th of April 2020, we conducted a survey through the popular Grahamstown/Makhanda Facebook Group and various local WhatsApp channels. This was one way of assisting us to design effective messaging for our community based on knowledge gaps of surveyed responses, as well as getting information out to people through trusted lines of communication. The survey focused on giving the team insight into the following areas:
1) current levels of concern around the pandemic
2) current areas of knowledge strengths and gaps with respect to COVID-19
3) practices known and being employed for personal and community safety
4) current sources of information and 'trusted' sources of information
5) preferred sources of information
6) reporting of prevalent myths circulated in the community and questions people would like to be addressed by scientists
We know that filling out surveys isn’t everyone’s idea of a good time, and we deeply appreciate the time taken by the 391 individuals who filled out the survey. As you can see from the activities we have been carrying out [see media repository page], the insights we gained from your activities have been put to good use in designing educational content and messages for the local community.
We would also like to share some feedback with you and answer some of the questions raised in the survey here. We will be updating this page regularly with further results, additional answers to your questions, and in line with new information as it emerges in the unfolding epidemic from reliable, open-access sources.
We know that not everyone in our Makana community was able to access or answer questions in an electronic survey. We would have liked to have come to speak to many of you in person to get your insights and questions, but this was not possible under the lockdown or from a public health perspective at the time. We hope that we will be able to do so in the future.
You can remind yourself of - or look at - the survey questions. Questionnaire-coronvavirus
The majority of participants who took the survey were in the age ranges of: 26-34 (19.7%) 35-49 (31.7%), and 50-65 (29.9 %).
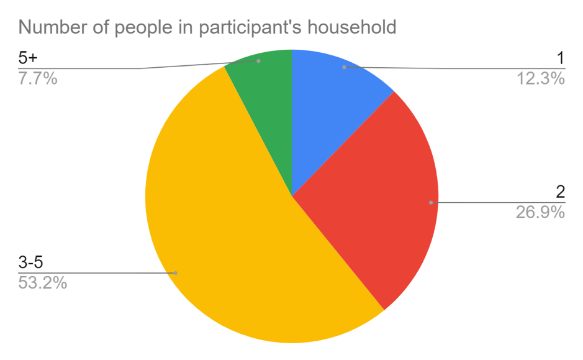
Only a small proportion of participants (12.3%) lived by themselves. More than half of the participants who took the survey (53.2%) live in households with 3-5 members.
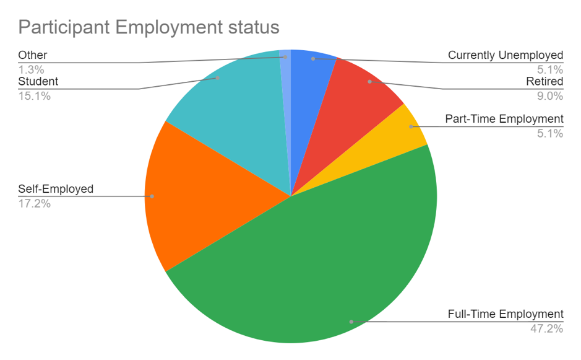
Students represented 15.1% of the survey respondents, while the majority of participants were either in full-time employment (47.2%) or self-employed (17.2%).
The following graph shows the results from participants in the survey who responded to the question ‘How worried are you about yourself and/or your family becoming infected with the coronavirus (COVID-19)?’. Only 3.6% of people who responded were not at all worried, while the majority (55%) of participants expressed high levels of concern (a score of either 4 or 5).
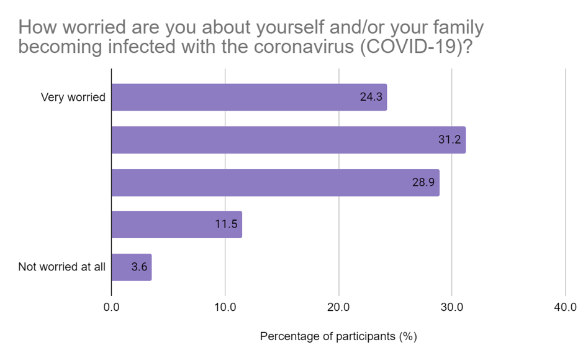
We have been faced with unrelenting news about the coronavirus pandemic and the numbers of infections and deaths caused by it. The virus has unquestionably had a serious impact on our day-to-day lives, and countless people have been affected economically, physically and emotionally. All of this does give us reason to be concerned and that is reflected in the results shown in the figure above. We should take the pandemic seriously.
At the same time, being anxious and on alert all the time can have a negative impact on mental and physical health. Using proven stress management techniques can be a vital resource in this time, and several guides to help can be accessed free online.
The Harvard Medical School has podcast lssons which are applicable to a broad range of life-circumstances and persons:
How to conquer your anxieties during the COVID-19 outbreak (Scroll down the page to access a series of podcasts).
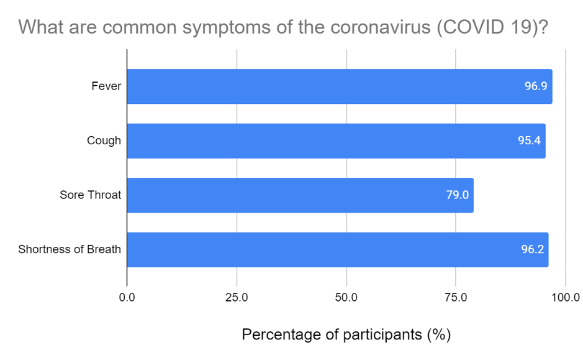
Participants in the survey were asked to identify the common coronavirus (COVID-19) symptoms, and the following graphs show the frequency of symptom selection or identification by participants.
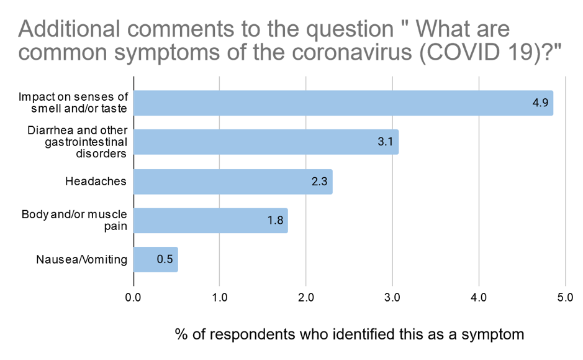
In the additional comments section of this question, participants also flagged the following as possible COVID-19 symptoms:
Coronavirus (COVID-19) most typically causes flu-like symptoms including a fever and a dry cough.
A sore throat, runny nose, and sneezing have only been observed in about 5% of patients infected with COVID-19. This was also the option that was least likely to be selected by a participant, probably due to the rareness of this symptom.
Similarly, diarrhea (which was identified as a symptom of COVID-19 by ~3.3% of respondents in the comments section) is also a symptom of COVID-19 infection. While only a few studies have been conducted on this symptom, a recent review of cases has concluded that gastrointestinal disorders are linked to COVID-19 infection, with between 3-79% of patients at various sites flagging these as symptoms. Of this class of symptoms, diarrhea is the most common symptom in both adults and children, while vomiting and nausea are most common in children.
After a week, COVID-19 infection can become severe in approximately 13.8% of cases, causing shortness of breath and pneumonia. Some of these cases can become critical, leading to respiratory failure, septic shock, and multi-organ failure in approximately 4.7% of all infections, or roughly a third of all severe cases.
Recent evidence is showing possible links between COVID-19 infection and a loss/alteration of senses of taste and smell in some patients. New evidence is emerging that severe cases may also be associated with increased risks of damage to the heart.
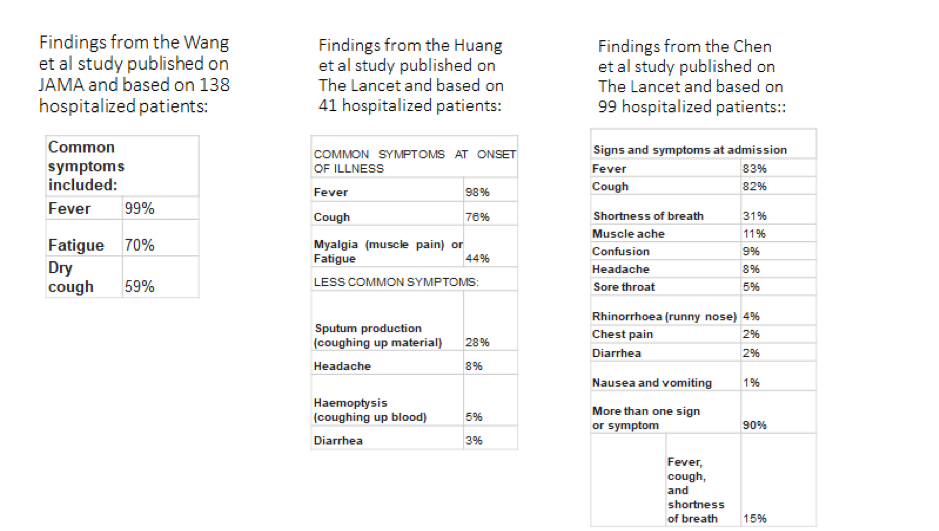
Studies from patients hospitalised with confirmed cases of COVID-19 (those representing severe to critical cases - around 20%) have reported observations of the following symptoms and their prevalence:
If you develop a high fever or persistent dry cough, speak to a medical advisor as soon as possible or call the free number: 0800 029 999. Take a coronavirus test if one is offered to you.
Sources:
Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China - JAMA, Wang et al., February 7, 2020
Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China - Huang et al., The Lancet. January 24, 2020
Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study - Chen et al, The Lancet, January 30, 2020
Symptoms of Novel Coronavirus (COVID-19) - United States Centers for Disease Control and Prevention (CDC)
Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Carol H. Yan, Farhoud Faraji, Divya P. Prajapati, Christine E. Boone, Adam S DeConde. International Forum of Allergy & Rhinology, 2020.
Heart Damage in COVID-19 Patients Puzzles Doctors. Up to one in five hospitalized patients have signs of heart injury. Cardiologists are trying to learn whether the virus attacks the organ. Hawryluk, M. Scientific American, April 6, 2020
Q&A on coronaviruses (COVID-19), WHO, 17 April 2020
Review article: gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Tian, Y. et al. Alimentary Pharmacology & Therapeutics, 2020 May; 51(9): 843–851.
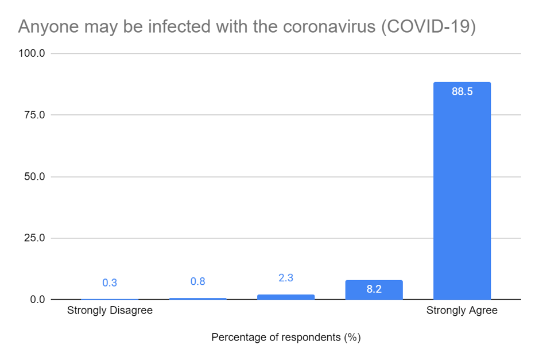
Participants in the survey were asked to what extent they agreed with the statement “Anyone may be infected with the coronavirus (COVID-19)”, and 88,5% of participants strongly agreed.
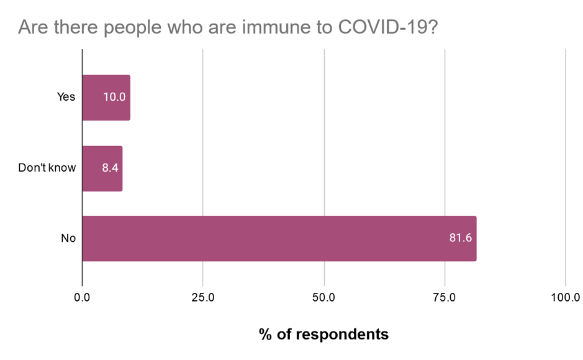
Participants were also asked if they thought there were people who were immune (could not become infected with) coronavirus: 81.6% of respondents to this question said no, while 8.4% said they were not sure or did not know, and 10% said yes. A large number of people (16.5% of participants) who said no speculated in their responses that patients who previously contracted COVID-19 may be immune from repeated infection by COVID-19.
Question six of the survey asked respondents to identify who they thought was most at risk of becoming seriously ill if they became infected with coronavirus (COVID-19). The following graphs show the frequency of potential high risk category selection or identification by participants.
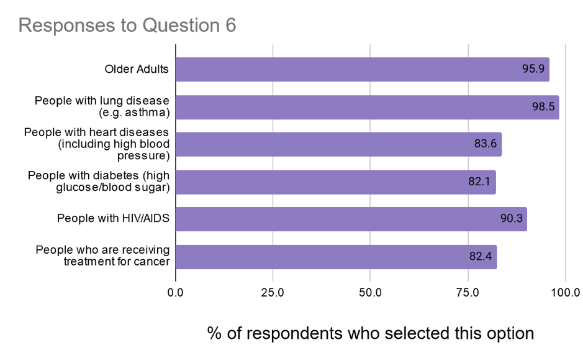
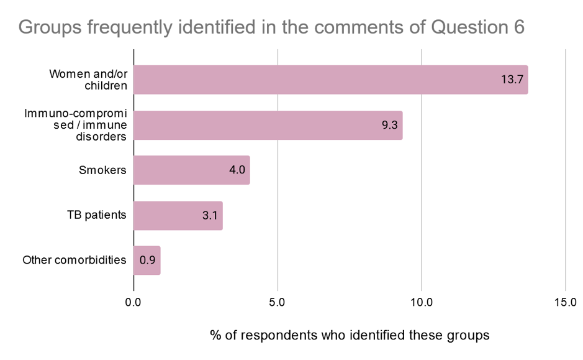
As additional comments, participants also identified the following groups as being at higher risk of contracting COVID-19:
The coronavirus pandemic has seen COVID-19 spread to 185 countries/regions. People from all countries can be infected.
Immunity to a disease can result when the immune system is triggered to produce antibodies to the disease in response to exposure. Immunity can be gained through infection by the disease - natural immunity - or through a vaccination which allows the body to produce antibodies through exposure to a weakened or dead form of the disease - vaccine-induced immunity.
Both natural immunity and vaccine-induced immunity can be long-lasting, even providing immunity for life in some cases, such as with the varicella virus (chickenpox). But immunity duration varies widely between diseases. Tetanus on the other hand requires regular booster vaccinations to maintain protection and natural infection offers no protection. We do not have a clear picture of where coronavirus (COVID-19) falls on the immunity spectrum relative to other diseases. It is not clear whether natural infection will offer protection or for how long yet. At the time of writing, the World Health Organisation does not believe there is enough evidence to equate having recovered from COVID-19 with being immune to reinfection.
Coronavirus can make anyone seriously ill, though there are factors which put some people at higher risk than others. Since COVID-19 is a novel virus, causing a new disease, we currently have a limited amount of information and data about the risk factors for severe illness resulting from infection.
Women, including pregnant women, have not been shown to be at higher risk of severe illness from COVID-19. The NHS (National Health Service, UK) has listed pregnant women as a vulnerable group as a precaution until more is known about the effects of COVID-19 and pregnancy, since in a small number of women the body's response in handling infection can be altered. Older men are reported to be slightly more likely to have an increased risk for severe illness resulting from infection. Of 72,314 cases reviewed by the Chinese Center for Disease Control and Prevention, less than 1% of the cases were in children younger than 10 years old, and most infected children appear to have a milder illness than adults.
According to the CDC (Centers for Disease Control and Prevention, USA), older adults, people aged 65 years and older, have an increased risk of severe illness. The NHS suggests that those over 70 are classified as being at high risk. The ECDC (European Centre for Disease Prevention and Control) reports that age specific hospitalisation rates show an increased risk for severe illness in those aged 60 and above, though the absolute number of deaths for those 65 and over is higher.
The options that were provided as selectable groups (older people, and those with underlying medical problems like high blood pressure, heart and lung problems, diabetes, or cancer) are those currently stated by the World Health Organisation as segments of the population that are at increased risk of contracting a serious case of COVID-19. Similarly, the CDC also identifies that people with underlying illnesses or medical conditions could be at a higher risk for severe illness. The CDC lists the following conditions and risk factors as potentially placing people at higher risk of severe infection from COVID-19:
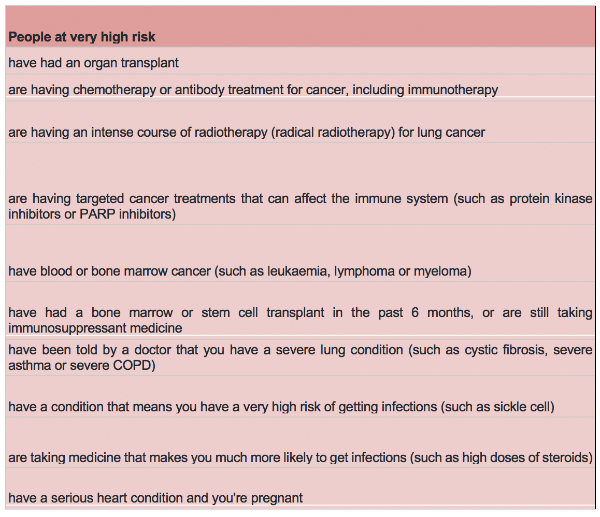
The NHS has advised two risk categories, high risk and very high risk, and suggests that those who are at very high risk take extra steps to protect themselves known as ‘shielding’, which includes not leaving home for any reason.
Sources:
Groups at Higher Risk for Severe Illness. CDC, USA.
Who's at higher risk from coronavirus. NHS, UK.
Coronavirus disease 2019 (COVID-19) in the EU/EEA and the UK – eighth update. ECDC, 8 April 2020.
General information and advice for all pregnant women during the coronavirus pandemic. Royal College of Obstetricians & Gynaecologists.
What Immunity to COVID-19 Really Means. McKenna, S. Scientific American April 10 2020.
Severe Acute Respiratory Syndrome Coronavirus 2−Specific Antibody Responses in Coronavirus Disease 2019 Patients.Okba, N. Emerging Infectious Diseases 26
A systematic review of antibody mediated immunity to coronaviruses: antibody kinetics, correlates of protection, and association of antibody responses with severity of disease. Cummings, D. et al.
"Immunity passports" in the context of COVID-19: Scientific Brief. WHO. 24 April 2020
SARS-CoV-2 Infection in Children. The New England Journal of Medicine. 2020; 382:1663-1665
"Immunity passports" in the context of COVID-19, Scientific Brief, WHO. 24 April 2020
Survey responses to the question ‘How is the coronavirus (COVID-19) transmitted between people?’. The following graphs show the frequency of possible transmission paths selected or identified by participants.
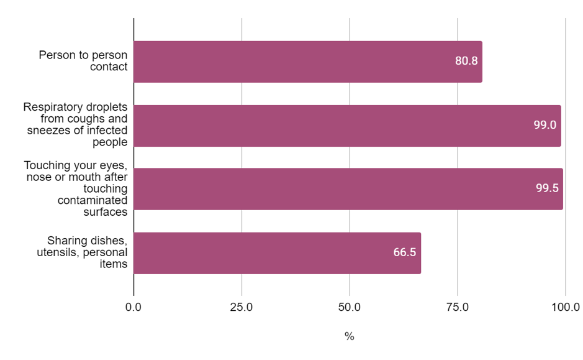
While the majority of respondents (>99%) identified that contact with respiratory droplets shed by infected people or shed onto contaminated surfaces transmitted COVID-19, significantly fewer participants selected either person to person contact or identified that sharing of eating utensils, dishes, or personal items might also transmit the virus.
The main way the coronavirus (COVID-19) spreads - mode of transmission - is from person to person.
The spread of coronavirus (COVID-19) between people occurs when respiratory droplets from an infected person land on the mouths, nose or eyes of another person, or are inhaled. Respiratory droplets can be produced when the infected person coughs, sneezes, spits, or talks.
After a short amount of time, these respiratory droplets land on surfaces since they are too heavy to remain airborne. By touching surfaces contaminated with respiratory droplets and then touching your eyes, nose, or mouth, you can introduce the virus into your system and become infected. The virus survives for different lengths of time on different surfaces; over time, the number of viable virus particles on any surface decreases and the possibility of infection is reduced. To minimize the potential spread avoid sharing toothbrushes, eating utensils, dishes, drinks, towels, washcloths or bed linen with other people if they have symptoms of coronavirus.
There have been no reports of COVID-19 transmission via food or food packaging, or postal packages.
Coronavirus (COVID-19) is not considered to be airborne, except under certain conditions in which aerosols-generating medical procedures are performed, such as during the intubation of a patient.
Both the virus genome and intact coronavirus (COVID-19) particles have been detected in stool samples of infected patients. However, it is not yet clear whether fecal-oral transmission is possible: to date, no cases involving fecal-oral transmission have been reported.
The best advice for slowing transmission is to maintain physical distancing - stay a few meters away from other people, cover your mouth and nose if you cough or sneeze.
Wash your hands often with soap and water for at least 20 seconds.
Do not touch your eyes, nose and mouth.
Sources:
Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief. WHO. 27 March 2020
Q&A on coronaviruses (COVID-19). WHO, 17 April 2020
Q & A on COVID-19. ECDC, 24 Apr 2020
What Should Gastroenterologists and Patients Know About COVID-19? Ungaro, R. et al. Clinical Gastroenterology and Hepatology 2020
COVID-19 and food safety: guidance for food businesses. WHO 7 April 2020
SARS-CoV-2 Isolation From Ocular Secretions of a Patient With COVID-19 in Italy With Prolonged Viral RNA Detection. Colavita, F. et al. Annals of Internal Medicine 17 April 2020
Coronavirus (COVID-19): What you need to know and learn. Unicef
Questions posed in the survey will be addressed in a separate webpage.
Last Modified: Thu, 07 May 2020 22:36:39 SAST