Whenever I am asked about the topic of my research, I tend to give a sigh (for a multitude of reasons) and then explain that I am studying women’s experiences of feticide from a critical health psychology perspective. Following the blank look on their face I tend to go on to explain the following:
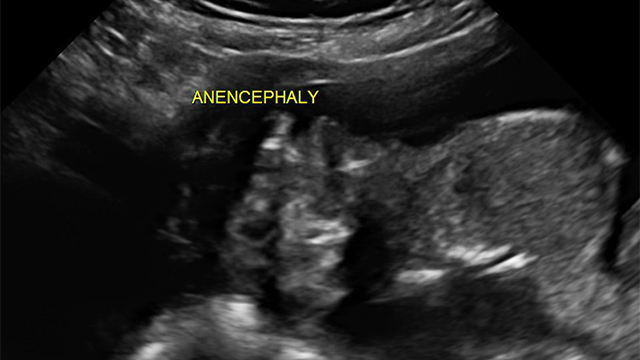
A number of congenital abnormalities are only detectable at advanced stages of gestation. In South Africa the late detection of abnormalities is increased by a lack of access to antenatal healthcare and delayed bookings at antenatal clinics. Foetal abnormality rates may also be increased due to greater instances of intrauterine infections, exposure to teratogens and maternal malnutrition in developing countries such as ours.
Late termination of pregnancy is legislated in South Africa by The Choice on Termination of Pregnancy Act (Act No.92 of 1996): if late termination is due to the presence of foetal abnormalities, it is legal at any gestational age. In South Africa the foetus has no legal status as a human and it is only following live birth that such status is conferred. Consequently, a complicating factor in late termination of pregnancy is the possibility that the foetus would survive the birth, and this is regarded as a ‘wrongful birth’. In order to avoid this medical and ethical dilemma from arising, the Royal College of Obstetricians and Gynaecologists advise a procedure called ‘feticide’ for all terminations of pregnancy later than 21 weeks and six days of gestation (earliest point of foetal viability). ‘Feticide’ is the process of causing fetal demise prior to birth by injecting potassium chloride into the foetal heart, causing cardiac arrest, or an intra-umbilical injection of potassium chloride or lignocaine in order to induce cardiac failure. Following this procedure, labour is induced and the foetus is stillborn.
South Africa has no guidelines or legislature on ‘feticide’, though medical consensus is that such decisions should be guided by a multi-disciplinary team. In South Africa the best interests of the pregnant woman prevail over the interests of the foetus prior to viability and she maintains the right to autonomy of choice regarding termination of pregnancy. Severe abnormalities are generally regarded as those likely to result in death or severe and irreversible deficits in cognitive development capacity - ‘incompatible with life’.
This is usually where I lose my audience entirely and tend to bear the brunt of horrified reactions. To some this is nothing short of eugenics. So who is acceptable enough to live and who is not? What conditions are truly ‘incompatible with life’ as we are so poor at predicting prognosis? Are women not better off not having to make this decision at all and instead carry all pregnancies full-term? Is it beneficial to end the pregnancy sooner rather than to witness the eventual demise of your child? These and so many more questions. So many varied reactions from sadness, to condemnation and anger.
Alas I can give no answers. I continue to interview women who have been through this procedure as well as the doctors who are involved with them. Will I have answers at the end of my thesis? I am not sure.
What I do know for sure, is that she who is furthest removed is most moral. We can never impose our decisions upon others because behind closed doors there are many more reasons for every decision than will ever be made known to others. Whether decisions are based on the lowest of Maslow’s needs, or the very highest, the pain involved in the loss and the collective and individual guilt do nothing to alleviate her suffering. However, the more we know about these procedures, the more we speak about them, the more we listen to women who have been through them; the more educated our opinions can be, the more empathy we can show and the less stigma there will be towards the women, their families and the medical staff involved.
